[ad_1]
In inflammatory bowel disorder, psychological anxiety can develop two painful responses
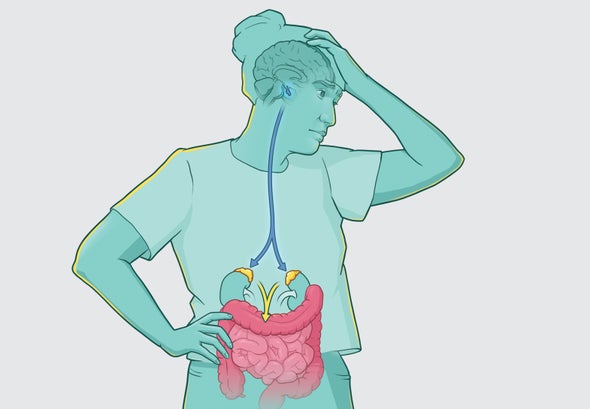
Bouts of disabling soreness, bleeding, fat loss and hospitalization that at times require operation: that is the ton of about 3 million adults in the U.S. who endure from inflammatory bowel disease, or IBD. (The illness has two key types, Crohn’s condition and ulcerative colitis. It is routinely linked with an overactive immune program and could have a genetic ingredient.) Remedies usually involve some variety of immunosuppressant these as a steroid drug. But even controlled circumstances have periodic flare-ups, and the explanations have been difficult to pin down.
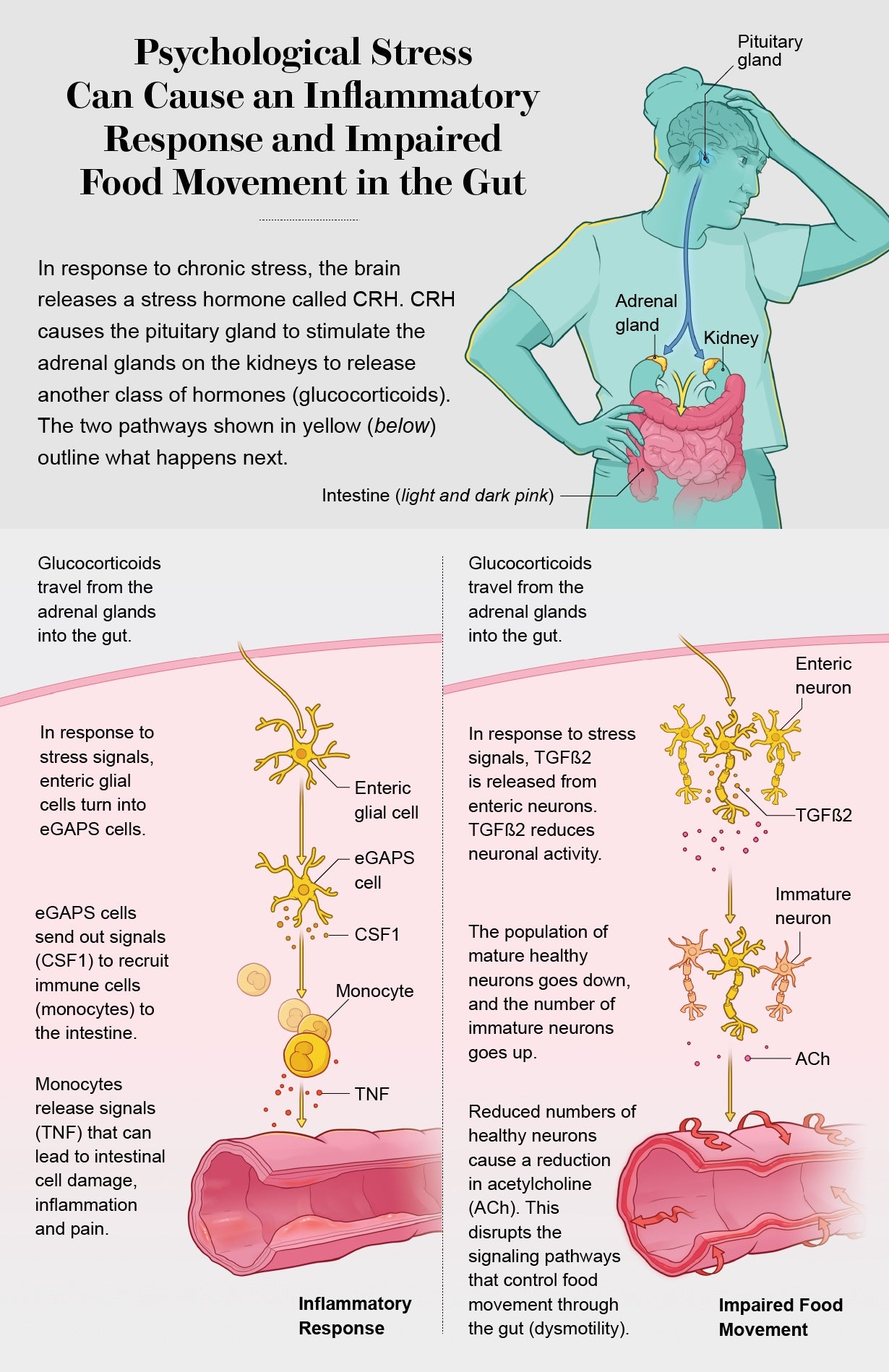
Now experts have traced two specific molecular pathways from the mind to the gut that develop IBD flares. And in three distinctive groups of IBD people, they discovered that psychological stress—a demise in the relatives or a poor combat with a loved just one, for instance—can result in the launch of mind substances that trigger IBD signs or symptoms. This isn’t going to mean IBD is all in the head, emphasizes Christoph A. Thaiss of the University of Pennsylvania, a person of the researchers. But it does indicate psychotherapy and focused strain-management techniques have important—and until finally now underappreciated—roles to play in avoiding and managing agonizing flares.


This post was originally released with the title “The Mind-Gut Relationship” in Scientific American 329, 2, 86 (September 2023)
doi:10.1038/scientificamerican0923-86
[ad_2]
Source backlink