[ad_1]
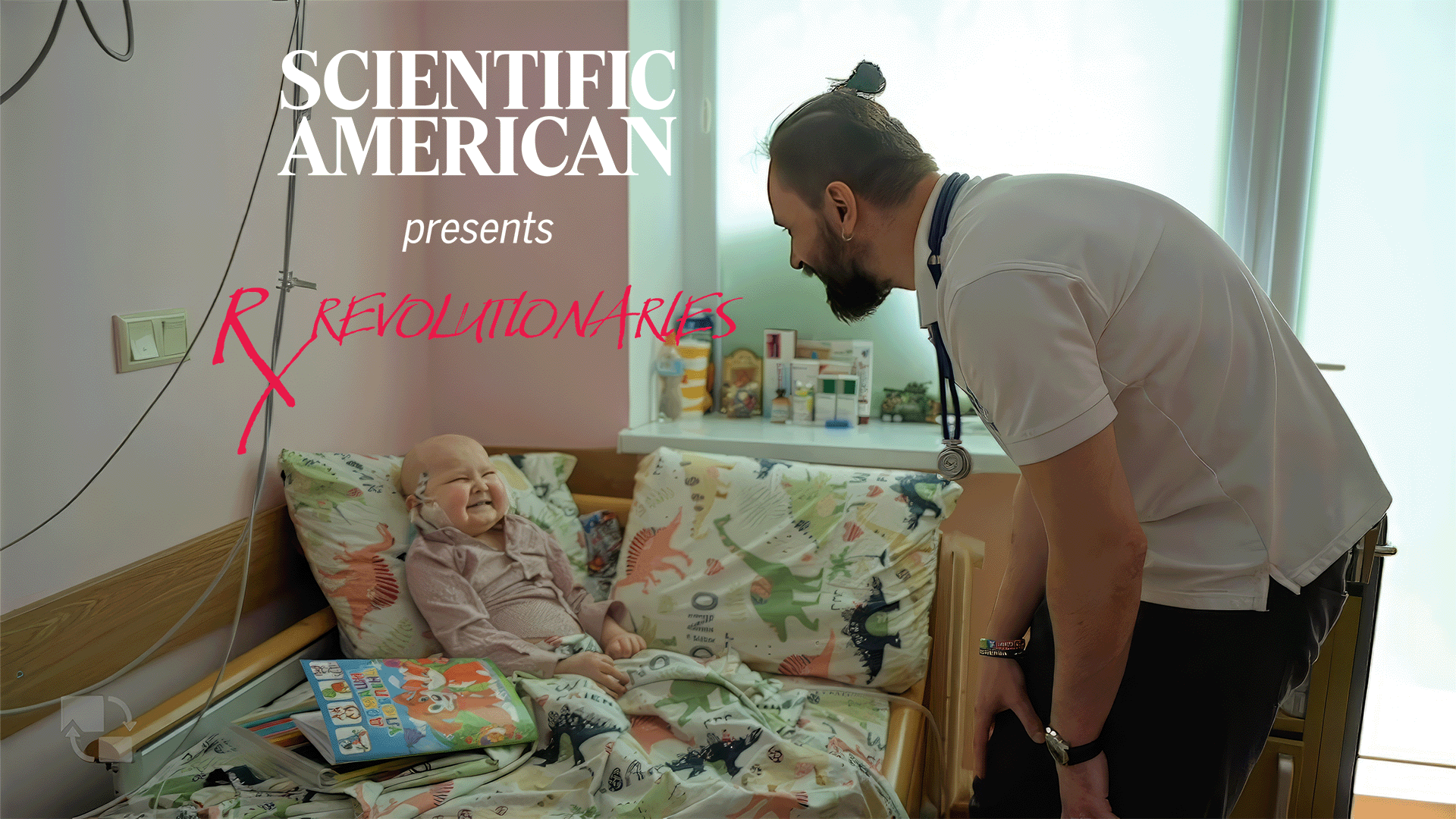
Roman Kizyma The to start with months of war, we failed to have the weekdays, so we just worked 7 times, 24 several hours.
There are times when I can operate for a few days with no snooze. There are moments like when I, I are not able to do anything for this day.
I experienced a pretty very long interval with out my incredibly modest young children. And so when I met in a pair of months, my more youthful son, so he didn’t understand me. So in comparison to the people that suffered the atrocities in Bucha or European or Eastern Ukraine, this is almost nothing. But this wasn’t a superior experience.
The main element for myself is this emotion of responsibility.
[Roman Kizyma, to camera] So when you see a bald dude or woman in the clinic, that is my patient.
If I just halt, I compromise the procedure of hundreds of little ones. And I imagine I am not in the place to to finish this.
[Roman Kizyma, in Ukrainian to patient] The place is the dilemma? Exactly where does it damage? Exhibit me.
[Patient] Here.
Roman Kizyma Here? Okay.
[Roman Kizyma in Ukrainian, to patient] Do you want to present me your tongue? Alright.
My name is Roman Kizyma. I am pediatric oncologist, a healthcare medical professional dealing with small children with most cancers. Now I’m the Performing Director of Western Ukrainian Specialised Children’s Professional medical Heart, a big, specialized hospital for seriously sick youngsters with cancer with other catastrophic illnesses.
The war made the issues for little ones with most cancers and other catastrophic sickness extremely challenging. You have to struggle two wars, one versus most cancers, the other against the nuts Russian military taking pictures at you. It is not only the actual physical unsafety, it’s also the complete disruption at some issue of professional medical logistics. So no medication coming to the medical center. No physicians or nurses obtainable in the direct clinic. The actual physical unsafety, the shelling of Ukrainian electricity infrastructure.
So often we have been black. All the hospital was black. No electrical power.
[Hospital staff, in Ukrainain] And our doctor’s don’t know this but
[Staff] — Oh everyone’s with flashlights.
[Hospital Staff singing Ukrainian National Anthem]
Roman Kizyma This is a susceptible group of patients. And when there is a form of crisis, vulnerable group of men and women suffers the most mainly because no a single cares. Absolutely everyone striving to preserve by themselves. So that’s why a lot of families like questioned or decided or went by by themselves to Europe with this job that we phone Safer Ukraine.
Right before the war, I was just dealing with most cancers. I transformed into somebody coordinating the large groups of pretty sick children likely listed here and there. So it signifies like a person and a half thousand children out of Ukraine with cancer taken care of someplace else. The team is ready to enable these young children and we have the ability. So which is why this is a unique hospital.
Through two years ahead of the start off of the war, we have been generating the new department, the Clinic of Pediatric oncology and stem mobile transplant below in this hospital.We opened this seven days right before the begin of the war, so we experienced a huge total of individuals heading to be addressed there. And we have to transform ourselves from oncologists to emergency medical doctors and relocate all our individuals to to to the other countries.
So it was a enormous blow for our stage of function. And we have to abandon all these new constructions that we established because you can not perform transplants when you are obtaining shellings and shootings and all these children.
[Roman Kizyma in Ukrainian] If not urgent then tomorrow, okay? Okay. If urgent I can seem now. Okay.
I feel so pressured. I sense like in a race against time. The relocation of a little one with most cancers from Ukraine to Western Europe is not a thing new. We did that even in advance of the war, but was like a pair of youngsters for every yr. But how do you do that if you have 100 children with cancer coming to your medical center per night.
These are severely ill kids. And for just about every of them you ought to have a whole lot of health care staff members to assistance each individual affected person.
[Nurse, in Ukrainian] Alright.
There is no clinic that can address 1,500 young children at a single time from some region. So this is not feasible,
[Child, in Ukrainian] It’s chilly.
Roman Kizyma That’s why we attempted to use different requirements. Very first of all, we structured multistep strategy with diverse hubs.
We acquired the requests from the households or the health professionals from various towns of the east of Ukraine or Kyiv, the funds. The initially hub is in Lviv. This medical center that can host any boy or girl of any severity. And if they simply cannot go further, we can treat them right here for a prolonged time or for a quick time and then allocate them.
We created with our partners, with charities or the guidance for housing and the capability for transportation. So we had a ton of volunteers conference kids in the railway station, carrying them out of there, carrying 20 individuals out of a coach in a railway station that is packed with men and women seeking to go somewhere. We went only [as] 5 medical professionals to meet a massive convoy at the railway station, so we have to carry youngsters throughout the railways.
The next action was the hub in Poland. The issue was to cross the border was a good deal of queues of folks hoping desperately to move out of Ukraine. So we made use of the diplomatic energy of Polish consulates situated in Lviv. This was preserving time for the severely ill little ones because if they stayed for 10 or 20 several hours in the queue, they would not depart it. So it was attainable.
In the future hub there was a triage of the international group that arrived listed here to Poland and they formed a logistics. A substantial resort was remodeled into a medical centre in the center of Poland. Small children were arriving there and they ended up triaged to different rooms and taken treatment by this team of worldwide health professionals.
Then they contacted their dedicated clinic all through Europe and U.SA and these hospitals and their government, they were transferring these youngsters to a particular clinic admitted by their crew. In the worst stage, we experienced extra than 150 young children for every 7 days despatched by this pathway. This was pretty hard.
[Roman Kizyma in Ukrainian, to patient] You can pull it up a little bit. Excellent.
Roman Kizyma My position was not to stage into just one into 1 scenario.
So this was I was oncologist myself. So I experimented with just to not to stage in each and every case additional than like 10 minutes. So I made use of my former expertise to triage them.
[Roman Kizyma in Ukrainian, to patient.] Fantastic. Can you smile? Can you smile and demonstrate your enamel? Superior, very well accomplished.
All through all these relocations, we lost two youngsters. It’s Russians who ended up attacking them, little ones have been from Kharkiv.
So it’s really near to the Russian border. That’s why throughout their incredibly critical cure stage, they had to be evacuated from their hospital, put into ordinary trains and they came to L’viv. Like we pretty much experienced no decision. So we experienced to describe to the families, you make your mind up what you do. You really don’t go and we continue to be and test to do something in this article in L’viv during these air strikes, or you risk.
But at the very least, you know you did everything to a little one. So they risked and we unsuccessful. So this both of those young children died. Some of their medical doctors who aided us listed here, they came from the areas that have been less than attack. There is a unfortunate story of our colleagues in Kyiv. 1 of their medical professionals, she was driving to her change for the young children with cancer.
She was strike straight by a Russian rocket in her car and she was burned alive. Her identify is Oksana Leontieva. And I consider this occasion, it was pretty influential. So we recognized how harmful, risky the do the job is.
[In Ukrainian, singing] Arms made some porridge and gave to Darynka. Jogging to get some porridge, Indeed.
But there were being a great deal of happy conditions. And I frequented a great deal of these hospitals later on, like in drop in the wintertime, that here. And the individuals had been joyful. The young children ended up joyful. Who are you treating? From time to time I felt like I was likely as a result of a medical center in Europe and like the initial place, my affected person, the second place, my patient. The 3rd space, my affected person.
So I was emotion like I’m the section of the staff of that clinic. You have been inquiring me like, What need to we do with your patients? So generally these are the great tales and the feedbacks the place like men and women are extremely grateful to all these nations around the world due to the fact they felt like they have been in residence. For the duration of last 12 months even as a pediatric oncologist, I assisted to build the services.
So I’ll consider to do that as a director, but not only for pediatric oncology, for instance, this will be the intensive care device, the big project in just this 12 months. So some men and women like outside of Ukraine, how can you make in the course of the wartime? You can. Why not? The lifetime even now goes on and we have to have these places for this severely sick little ones that will glimpse greater.
So that is what I am concentrated now to to do that. This is a community that check out to stability alone. So this is a never ever ending system. I hope this will do the job.
[The above is a transcript of this podcast]
[ad_2]
Source website link